In addition to lowering blood pressure, this gentle form of exercise can help maintain strength, balance, flexibility and mental health and is an ideal activity for all ages!
This research was brought to my attention by my friend and mentor from Dalton, Peter Frieder, Chairman,Gentex Corporation and current Board Chair at WVIA. Peter is celebrating his birthday today with a number of years that clearly does not represent his physiological age, in great part due to his dedication to health and wellness. Happy Birthday and thank you!
According to a new study by the China Academy of Chinese Medical Sciences (CACMS), the ancient martial art practice of Tai Chi is effective in lowering blood pressure as much, if not more, than traditional aerobic exercise. For those with prehypertension or hypertension and are unable to tolerate the repetitive and prolonged weight bearing stresses of running, walking or cycling, these results have tremendous implications. The slow, gentle and controlled movements and positions of Tai Chi coupled with controlled breathing and meditation may be a valuable alternative, especially for those with aging muscles and joints. Improved strength, flexibility balance, posture and mental health are additional bonuses.
Tai Chi is multifaceted in that it combines martial arts, slow gentle and controlled movements, sustained postures, a focused and meditative mind, and controlled breathing. It is considered by many to be “meditation or medication in motion.”
Tai Chi involves slow-motion movements transitioning with control from one position to another. The positions have historically been named for the actions of animals, for example:

Deep and purposeful breathing, mental focus, body awareness and meditation are integral components of the exercise. The beauty of Tai Chi is not only in the physical form, but also in its safety for all levels of fitness. It is helpful for individuals from high level athletes to those with physical disabilities. The movements are natural and gentle without forcing the muscles and joints to extreme or uncomfortable positions. It is often used as an adjunct therapy in the wellness as well as rehabilitation of a variety of athletic (ACL surgery, joint replacements) and neurological conditions (Parkinson’s, MS, head trauma), to name a few. Based on the aforementioned Chinese study, Tia Chi can be applied as a technique to control or lower blood pressure, especially for those who cannot utilize traditional aerobic exercise.
Tai Chi has been found to offer many physical and mental benefits. Some of these include:
Muscle Strength – upper and lower body, trunk and core strength
Flexibility – participants report improved range of motion and flexibility of the spine and extremities
Balance and Proprioception – some studies report a reduction of falls due to a variety of sustained positionsand improved awareness of one’s body in space
Aerobic Conditioning - recent studies have found that participants have lower heart rate and blood pressure
Mental Health – through improved balance, strength, and flexibility, studies show participants have gained confidence and control as well as lower blood pressure and stress reduction.
All Tai Chi classes begin with four basic principles: warm-up, instruction, practice and breathing.
Warm-up- gentle easy motions to warm-up and loosen the joints and muscles to prevent injury.
Tai Chi Forms – “Short Forms” are beginner movements which are gentle, slow, and short in duration while “Long Forms” are more advanced.
Breath Work – gentle breathing combined with movement to relax the mind and focus energy
Don’t be intimidated by the language or history – Yang, Wu, Cheng are only brands of movements with a history of martial arts but this in no way impacts participation.
Get medical clearance – check with your physician to see if Tai Chi is safe for you. Some orthopedic or vestibular problems might require special attention.
Observe or take a beginner class – often available at local fitness clubs or senior centers. Research options in your area and find a friend to join you. Consider an introductory instructional video to get a feel for Tai Chi. (See local Tia Chi classes below)
Meet with an instructor – if it makes you more comfortable, make time to talk to an instructor before enrolling in a class.
Dress for success – wear loose-fitting clothes that allow for range of motion and comfortable shoes for balance and support.
Track your progress – use an app or keep a journal of your progress. Heart rate, blood pressure and endurance (the time you can hold a pose or tolerate a class) are easy to monitor.
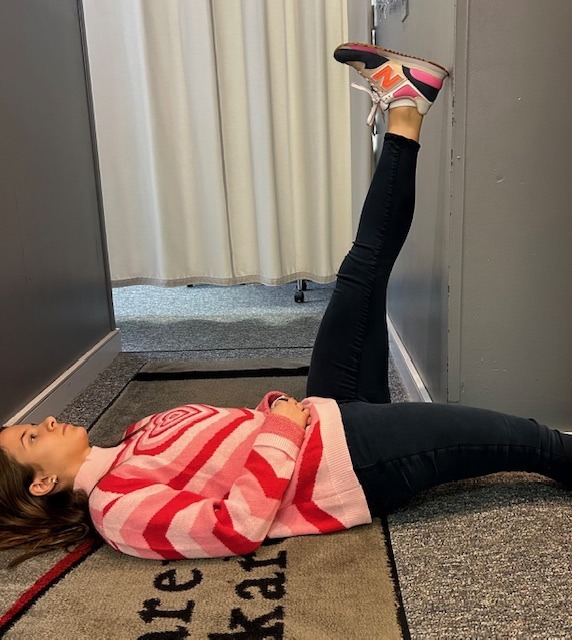
Model: Lily Smith, University of Scranton Physical Therapy Student and PT aide at Mackarey Physical Therapy.
Sources: HarvardHealthPublishing; New Atlas; China Academy of Chinese Medical Sciences (CACMS); National Institutes of Health
Local Tai Chi Classes: Steamtown Yoga, Scranton, PA; Mission Yoga, Scranton, PA;Dragon’s Heart Tai Chi & Kung Fu, Clarks Summit, PA; Rothrocks Kung Fu & Tai Chi, Duryea, PA
For more information: HarvardHealth; www.taichihealth.com; www.treeoflifetaichi.com

EVERY MONDAY – Read Dr. Paul J. Mackarey “Health & Exercise Forum!” via Blog
EVERY SUNDAY in "The Sunday Times" - Read Dr. Paul J. Mackarey “Health & Exercise Forum!” in hard copy
This article is not intended as a substitute for medical treatment. If you have questions related to your medical condition, please contact your family physician. For further inquires related to this topic email: drpmackarey@msn.com
Paul J. Mackarey PT, DHSc, OCS is a Doctor in Health Sciences specializing in orthopaedic and sports physical therapy in Scranton and Clarks Summit. Dr. Mackarey is in private practice and is an associate professor of clinical medicine at Geisinger Commonwealth School of Medicine. For all of Dr. Mackarey's articles, visit our exercise forum!
Seasonal allergies affect 30 % of adults and 40% of children in the United States. Avoiding the outdoors is often not an option…especially if you enjoy outdoor activities and sports. Not long ago, it was unthinkable that an athlete with serious seasonal allergies could compete at a high level, such as the Olympics. Now, in great part due to advanced research, medications and proper management, an Olympic gold medal for those suffering from seasonal allergies is a reality. Recently, the National Institute of Allergy and Infectious Disease at the National Institutes of Health have published research on this topic to provide a better understanding and make recommendations.
The most common allergic reactions which athletes suffer from are sneezing, itchy and watery eyes, runny nose and coughing. Moreover, 67% of those with these symptoms also suffer from asthma. The athlete in NEPA is particularly vulnerable when the pollen count is high during spring and fall for several reasons. One, after being indoors all winter, one might develop a heightened sensitivity to allergens. Also, increased rapid and deep breathing during exercise makes athletes more susceptible to significant symptoms when exposed to allergens such as tree, grass and weed pollens.
Allergy skin testing can be performed to determine the allergens to which you are susceptible. Once determined, allergy shots are effective in building up tolerance to these allergens. If appropriate, you may be able to use allergy drops, administered under the tongue and conveniently used at home.
Asthma suffers should use their inhaler BEFORE symptoms occur. A recent study found that pretreatment using a short-acting bronchodilator inhaler within 15 minutes before exercise is very effective in preventing asthma symptoms for more than four hours. It is important to keep a bronchodilator available. If you fail to benefit from this, see your physician for other methods to control your exercise-induced symptoms.
Whether you have allergic respiratory problems from rhinitis or asthma, you many benefit from conditioning your airways with a 10 to 15 minute warm-up before and cool-down after the activity. This may serve to gradually prepare your lungs for an increased demand.
In addition to preventing dehydration on hot and humid days, constant hydration is very important for the athlete with allergies to prevent dry airways in athletes.
Know the signs and symptoms of asthma (coughing, wheezing, tightness in chest, shortness of breath).
Some schools have a file on each student athlete with a allergic or asthmatic problem which requires medication. The file includes information such as medical doctor release and instruction, emergency contacts and medications. Students must have their medications on hand before they can enter the field. The National Athletic Trainers Association recommends using a peak flow meter to monitor at risk players and can determine when a player can return to the field.
If possible, find an alternate practice facility with climate control for athletes at risk. Plan practices for these athletes when the pollen count is low. Check the newspaper or internet for pollen counts in your area. Training by the water, (ocean) where there is a breeze and less pollen is helpful.
Shower and change clothing immediately after being outdoors
During a flare up, do less aerobic exercise to limit stress on respiratory system. Try strength training indoors instead.
When pollen count is high, keep windows shut at home and in your car….use air-conditioning.
Keep pets out of your bedroom…especially when sleeping
Dry clothing in dryer…do not hang on clothesline outdoors
Sources: American College of Allergy, Asthma, and Immunology. National Athletic Trainers Association.

EVERY MONDAY – Read Dr. Paul J. Mackarey “Health & Exercise Forum!” via Blog
EVERY SUNDAY in "The Sunday Times" - Read Dr. Paul J. Mackarey “Health & Exercise Forum!” in hard copy
This article is not intended as a substitute for medical treatment. If you have questions related to your medical condition, please contact your family physician. For further inquires related to this topic email: drpmackarey@msn.com
Paul J. Mackarey PT, DHSc, OCS is a Doctor in Health Sciences specializing in orthopaedic and sports physical therapy in Scranton and Clarks Summit. Dr. Mackarey is in private practice and is an associate professor of clinical medicine at Geisinger Commonwealth School of Medicine. For all of Dr. Mackarey's articles, visit our exercise forum!
This column is dedicated to the memory of John R. O’Brien, Esq., who recently passed due to medical complications associated with multiple sclerosis (MS). John was a source of joy and inspiration for those fortunate to have known him. Twenty years ago, John hesitantly agreed to contribute to my column on MS with two requirements: one, if the column would be valuable to those affected by MS and two, he would remain anonymous. When speaking with his dedicated wife, Sally, it became very apparent that any discussion of John’s life would be diminished if it was defined by the disease because he was committed to turning his “DISABILITY INTO AN ABILITY!”
With the help of his loving wife, family, friends, and devices such as an electric scooter and adaptive car, John not only lived but thrived! He was a skilled lawyer, a respected member of the Bar, and an active member of the community. John served on the executive committee of the Lackawanna Bar Association. In addition, the Lackawanna Pro Bono honored him recently. He also taught business law and healthcare law and coached Prep’s mock trial team.
John shared his thoughts with me about the challenges of redefining life… from Golf Club Champion to living with a physically disabling disease. Anyone who knew him would agree that he succeeded in doing so through his keen intellect and sharp wit and humor…his heart and brain overcompensated for his body! In addition to reading books in Latin and Greek, he had his crossword puzzles published in The New York Times and Los Angeles Times. In September 2023, John conducted an interview with presidential historian Doris Kearns Goodwin before a full house at the Scranton Cultural Center. Ms. Goodwin later reported that John was the most knowledgeable, effective and enjoyable interviewer she’s encountered.
John’s absence will be deeply felt and his legacy will continue to shape our community for years to come!
Multiple Sclerosis is a chronic disease. While it may lay dormant and stable for a period of time, living a healthy lifestyle will make a positive contribution toward how you and your family live with Multiple Sclerosis. Studies show that a life of family, love, and support are essential to maintain a positive attitude with a chronic illness. This combined with a healthy diet and proper exercise can contribute greatly toward taking control and living a relatively normal life with MS.
As I have mentioned in many other columns, studies show that people with good attitudes and great faith live longer than others. This is especially helpful when living with chronic disease like Multiple Sclerosis. The Cleveland Clinic offers some suggestions how to maintain a positive attitude:
Many sources, including the Cleveland Clinic suggest that exercise, when performed properly, can have a positive impact on Multiple Sclerosis symptoms both physically and psychologically. However, because you have a chronic illness, you should consult with you family physician and physical therapist before beginning an exercise program. They will advise you on the proper type and amount of exercise.

EVERY MONDAY – Read Dr. Paul J. Mackarey “Health & Exercise Forum!” via Blog
EVERY SUNDAY in "The Sunday Times" - Read Dr. Paul J. Mackarey “Health & Exercise Forum!” in hard copy
This article is not intended as a substitute for medical treatment. If you have questions related to your medical condition, please contact your family physician. For further inquires related to this topic email: drpmackarey@msn.com
Paul J. Mackarey PT, DHSc, OCS is a Doctor in Health Sciences specializing in orthopaedic and sports physical therapy in Scranton and Clarks Summit. Dr. Mackarey is in private practice and is an associate professor of clinical medicine at Geisinger Commonwealth School of Medicine. For all of Dr. Mackarey's articles, visit our exercise forum!
This column is dedicated to the memory of John R. O’Brien, Esq., who recently passed due to medical complications associated with multiple sclerosis (MS). John was a source of joy and inspiration for those fortunate to have known him. Twenty years ago, John hesitantly agreed to contribute to my column on MS with two requirements: one, if the column would be valuable to those affected by MS and two, he would remain anonymous. When speaking with his dedicated wife, Sally, it became very apparent that any discussion of John’s life would be diminished if it was defined by the disease because he was committed to turning his “DISABILITY INTO AN ABILITY!”
With the help of his loving wife, family, friends, and devices such as an electric scooter and adaptive car, John not only lived but thrived! He was a skilled lawyer, a respected member of the Bar, and an active member of the community. John served on the executive committee of the Lackawanna Bar Association and was recently honored by the Lackawanna Pro Bono. He also taught business law and healthcare law and coached Prep’s mock trial team.
John shared his thoughts with me about the challenges of redefining life… from Golf Club Champion to living with a physically disabling disease. Anyone who knew him would agree that he succeeded in doing so through his keen intellect and sharp wit and humor…his heart and brain overcompensated for his body! In addition to reading books in Latin and Greek, he had his crossword puzzles published in The New York Times and Los Angeles Times. In September 2023, John conducted an interview with presidential historian Doris Kearns Goodwin before a full house at the Scranton Cultural Center. Ms. Goodwin later reported that John was the most knowledgeable, effective and enjoyable interviewer she’s encountered.
John’s absence will be deeply felt and his legacy will continue to shape our community for years to come!
According to the National Multiple Sclerosis Society, Multiple Sclerosis affects approximately 400,000 people in the United States. Multiple Sclerosis is second only to trauma as the most common cause of neurological disability for those in early to middle adulthood. MS is almost three times as common in women. Multiple Sclerosis is very uncommon before adolescence or after 50. However, the risk increases from teen years to age 50.
Multiple sclerosis is considered to be an autoimmune disease. The immune system of the body does not work properly when it fails to attack and protect the body against substances foreign to the body such as bacteria. Instead, the system allows the body to attack normal tissues and create diseases such as MS, rheumatoid arthritis and lupus.
In MS, the immune system attacks the brain and spinal cord of the central nervous system. Each nerve has an outer covering of a fatty material (myelin) for insulation to improve the transmission and conductivity of impulses or messages to and from the brain. The damage to the myelin of the nervous system interrupts the ability of messages to travel to and from the brain, through the spinal cord and to other areas of the body such as the muscles in the arms and legs. Due to this “short circuiting” the brain becomes unable to send or receive messages. In multiple sclerosis, scar tissue or plaques (sclerosis) replaces the fatty myelin in “multiple” areas. This is also called demyelination.
The symptoms associated with MS vary greatly from person to person. The amount, frequency and speed of the demyelination process vary greatly and are directly related to the loss of strength and function in daily activities. Some people are independent and ambulatory with mild and infrequent episodes of weakness and disability and live a relatively normal life. Others suffer from frequent and aggressive episodes that significantly weaken and disable. Some common symptoms in the early stages include: muscle weakness, loss of coordination, blurred vision, pain in the eyes, double vision. Some common symptoms as the disease progresses are: muscle stiffness with muscle spasms, pain, difficulty controlling urination, difficulty thinking clearly.
The diagnosis of MS can be very difficulty in the early stages because the symptoms are often vague and temporary. Also, MS symptoms are very similar to other neurological problems. A neurologist will run several tests to rule out other possible problems. However, an MRI showing demyelination of the nerves is a primary confirmation.
Treatment for MS depends upon many factors and requires consultation with your physician. Some medications can control the frequency and severity of MS symptoms such as pain, weakness, and spasticity. Also, some drugs can slow the progression of certain types of MS. Additional treatments for MS include: diet, exercise, physical therapy, support groups, and counseling for the MS patient and their family. Part II of Multiple Sclerosis will discuss these options in further detail next week.
Visit your doctor regularly and listen to your body.

EVERY MONDAY – Read Dr. Paul J. Mackarey “Health & Exercise Forum!” via Blog
EVERY SUNDAY in "The Sunday Times" - Read Dr. Paul J. Mackarey “Health & Exercise Forum!” in hard copy - NEXT WEEK: PART II OF II - MULTIPLE SCLEROSIS
This article is not intended as a substitute for medical treatment. If you have questions related to your medical condition, please contact your family physician. For further inquires related to this topic email: drpmackarey@msn.com
Paul J. Mackarey PT, DHSc, OCS is a Doctor in Health Sciences specializing in orthopaedic and sports physical therapy in Scranton and Clarks Summit. Dr. Mackarey is in private practice and is an associate professor of clinical medicine at Geisinger Commonwealth School of Medicine. For all of Dr. Mackarey's articles, visit our exercise forum!
A myth is a traditional story, idea, or belief, especially one concerning early history of a people or explaining a natural or social phenomenon. It is a widely held but false belief or idea. In medicine, health myths are also widely held beliefs about health issues such as medicines, herbs, treatments, cures, antidotes, etc. which are partially or totally false and unsubstantiated in the scientific literature. This is a partial list of the most common health myths:
SOURCES: WebMd; National Institutes of Health, Mayo Clinic

EVERY MONDAY – Read Dr. Paul J. Mackarey “Health & Exercise Forum!” via Blog
EVERY SUNDAY in "The Sunday Times" - Read Dr. Paul J. Mackarey “Health & Exercise Forum!” in hard copy
This article does not intend as a substitute for medical treatment. If you have questions related to your medical condition, please contact your family physician. For further inquires related to this topic email: drpmackarey@msn.com
Paul J. Mackarey PT, DHSc, OCS is a Doctor in Health Sciences specializing in orthopaedic and sports physical therapy in Scranton and Clarks Summit. Dr. Mackarey is in private practice and is an associate professor of clinical medicine at Geisinger Commonwealth School of Medicine. For all of Dr. Mackarey's articles, visit our exercise forum!
PEOPLE OFTEN ASK ME, “IS THERE SUCH A THING AS AN EXERCISE RUT?”. THEY WANT TO KNOW WHY THEY DO NOT SEEM TO BE IMPROVING WITH THEIR EXERCISE PROGRAM. They exercise 3-4 times a week for 30 to 45 minutes and they feel frustrated and STUCK in a rut.
The purpose of this column is to offer suggestions to improve or get more out of a “stale” exercise program. Last week’s column offered tips to improve a stale cardiovascular and strength program. We will discuss flexibility and functional training tips, including the components necessary for a healthy mind, body and spirit connection.
Flexibility training involves the careful stretching of the muscles, tendons and joints to improve range of motion in order to safely perform daily activities and sports without injuring or tearing soft tissues. It is probably the most neglected part of the fitness program. However, while the amount of inherent flexibility varies for each person, a minimal range is necessary as it relates to daily activities and sports. For example, as you age it is important to have enough flexibility in your back, hips and knees to wash your feet, put shoes and socks on. After a warm –up activity, perform flexibility exercises slowly and gently. There are two types of flexibility exercises; dynamic and static. Perform dynamic stretching with movement such as pushing the ankle up and down like a gas pedal. Complete passive stretching using an outside force, such as a towel to pull the ankle up to stretch the calf. Dynamic should be performed before an activity (before running or playing tennis) and static performed after the activity is over in order to increase range of motion for future activities.

In order to prevent an exercise program from getting stale, one must incorporate all aspects of wellness…a healthy mind, body and spirit!
It is easy for fitness enthusiasts to get so focused on maintaining a routine that they allow their program to become stale and ineffective. It is essential to reassess and update your program to prevent stagnation.
Make sure the routine has all three fundamental components of a well-balanced exercise program; cardiovascular, strength and flexibility training. Moreover, to be truly healthy, one must work toward a “Healthy Mind, Body, and Spirit. Therefore, in addition to traditional exercise one must incorporate the following: nutrition; meditation, relaxation techniques, yoga, core fitness; functional/sports specific training; leisure sports and activities
In order to prevent an exercise program from getting stale, one must incorporate all aspects of wellness…a healthy mind, body and spirit!
While each component offers its own specific benefit, the combination of all three cooperatively provides unique value. Too often, fitness enthusiasts concentrate on the exercises they LIKE or are good at more than the ones they NEED.
Sources: National Institutes of Health; American Council on Exercise
Model: Lily Smith, Physical Therapy Student, University of Scranton, PT aide, Mackarey Physical Therapy

EVERY MONDAY – Read Dr. Paul J. Mackarey “Health & Exercise Forum!” via Blog
EVERY SUNDAY in "The Sunday Times" - Read Dr. Paul J. Mackarey “Health & Exercise Forum!” in hard copy
This article is not intended as a substitute for medical treatment. If you have questions related to your medical condition, please contact your family physician. For further inquires related to this topic email: drpmackarey@msn.com
Paul J. Mackarey PT, DHSc, OCS is a Doctor in Health Sciences specializing in orthopaedic and sports physical therapy in Scranton and Clarks Summit. Dr. Mackarey is in private practice and is an associate professor of clinical medicine at Geisinger Commonwealth School of Medicine. For all of Dr. Mackarey's articles, visit our exercise forum!
PEOPLE WILL OFTEN ASK ME, “IS THERE SUCH A THING AS AN EXERCISE RUT?” THEY WANT TO KNOW WHY THEY DO NOT SEEM TO BE IMPROVING WITH THEIR EXERCISE PROGRAM…they exercise 3-4 times a week for 30 to 45 minutes and they feel frustrated and STUCK in a rut. While initially responding favorably to exercise, after 6 -9 months or more, they do not notice progress in weight loss, strength, tone, endurance or daily function.
The purpose of this column will be to offer suggestions on how to improve or get more out of a “stale” exercise program or an exercise rut. Step one is to build an exercise program that is grounded in the basics. Next step two, which begins after the basics have been mastered, includes the components necessary for a healthy mind, body and spirit connection and translates into functional activities of daily living including work and leisure sports.
Make sure your routine has all three fundamental components of a well-balanced exercise program; cardiovascular, strength and flexibility training. While each component offers its own specific benefit, the combination of all three cooperatively provides unique value. Too often, fitness enthusiasts concentrate on the exercises they LIKE or are good at more than the ones they NEED. A well-balanced program includes what you like and need! In fact, recent studies show that those performing all three components surpassed those performing one or any combination of two of the training types when tested for efficient oxygen uptake (VO2 Max), production of HDL (good cholesterol), lower body fat percentage, and lower blood glucose levels.
Cardiovascular exercise is any activity that raises your heart rate and respiratory rate. This type of exercise strengthens the heart muscle and the muscles that assist in breathing. When these muscles are stronger, they in turn work more efficiently to deliver oxygen to your muscles and other parts of the body. Ultimately, these oxygenated muscles can work harder and longer to burn fat during exercise and at rest.
Examples of Cardiovascular Exercises: Running, Brisk Walking, Swimming, Biking, Rowing, Elliptical Training and Stepper Training. Most experts recommend at least 30 minutes of sustained cardio, 3-4 days per week. However, recent studies support the notion of performing 10-15 minutes, twice daily, 4 days per week. For those “stuck” in a fitness or exercise rut, to advance your program, cardio should be performed 5-6 days per week for 45-60 minutes.
Strength training is an activity that provides any type of resistance to muscle contraction to build strength in the muscle. The resistance can be without movement against an immovable object such as pushing against a wall (isometric) or with movement such as lifting up or lowering a weight down against gravity (isotonic/dynamic). There are two types of isotonic muscle contraction; concentric, which involves raising the weight against gravity as the muscle shortens and eccentric which involves lowering a weight against gravity as the muscle lengthens. A standing biceps curl is an example that incorporates both concentric and eccentric contractions. A progressive strength training program includes all three types of muscle contraction. By using the classic bicep muscle curl these photos will demonstrate all three types of muscle contraction:
-Isometric Bicep Muscle Curl – pull up on door knob without allowing any movement of the arm.
-Concentric Bicep Muscle Curl – raise a dumbbell up against gravity as the muscle shortens.
-Eccentric Bicep Muscle Curl – lower a dumbbell slowly (4-6 seconds) against gravity as the muscle lengthens.
Sources: National Institutes of Health; American Council on Exercise

EVERY MONDAY – Read Dr. Paul J. Mackarey “Health & Exercise Forum!” via Blog
EVERY SUNDAY in "The Sunday Times" - Read Dr. Paul J. Mackarey “Health & Exercise Forum!” in hard copy
NEXT WEEK! Read Stuck in an Exercise Rut…Part II of II:
This article is not intended as a substitute for medical treatment. If you have questions related to your medical condition, please contact your family physician. For further inquires related to this topic email: drpmackarey@msn.com
Paul J. Mackarey PT, DHSc, OCS is a Doctor in Health Sciences specializing in orthopaedic and sports physical therapy in Scranton and Clarks Summit. Dr. Mackarey is in private practice and is an associate professor of clinical medicine at Geisinger Commonwealth School of Medicine. For all of Dr. Mackarey's articles, visit our exercise forum!
February is National Cancer Prevention Month and March is Colorectal Cancer Awareness Month. Unfortunately, according to a study conducted by Northeast Regional Cancer Institute (NRCI), our area has a higher rate of cancer compared to the rest of the United States. Residents of NEPA must be vigilant! While there is no fool-proof method for cancer prevention, scientific research does support the fact that healthy lifestyle choices are essential.
Source: American Cancer Society

EVERY MONDAY – Read Dr. Paul J. Mackarey “Health & Exercise Forum!” via Blog
EVERY SUNDAY in "The Sunday Times" - Read Dr. Paul J. Mackarey “Health & Exercise Forum!” in hard copy
This article is not intended as a substitute for medical treatment. If you have questions related to your medical condition, please contact your family physician. For further inquires related to this topic email: drpmackarey@msn.com
Paul J. Mackarey PT, DHSc, OCS is a Doctor in Health Sciences specializing in orthopaedic and sports physical therapy in Scranton and Clarks Summit. Dr. Mackarey is in private practice and is an associate professor of clinical medicine at Geisinger Commonwealth School of Medicine. For all of Dr. Mackarey's articles, visit our exercise forum!
I enjoy the privilege of working with people recovering from a wide variety of medical conditions. Many of these conditions can directly affect activities of daily living, particularly, the ability to drive safely: orthopedic and sports injuries, fractures, sprains and strains, joint replacements, hip fractures, shoulder and elbow surgeries and spinal fusions. Despite the many different types of problems, there is one question that is invariably asked, “When can I return to driving?” Unfortunately, the answer is not as simple as the question because it depends on many factors. Furthermore, the implications, such as a serious accident causing further damage to the injury or surgical site or harm to someone else, are significant and possibly critical. So, the next time you ask your physician this question, please follow instructions and be patient…remember, it could be your child or grandchild running into traffic to chase a ball and you would want the driver to be at optimal function to apply the brakes!
In our culture, the inability to drive has a significant impact on lifestyle and livelihood. A study published in the Journal of Bone and Joint Surgery, found that 74% of those unable to drive due to injury or surgery are dependent on family and most of the remainder depend on friends. 4% of those unable to drive have no help at all and more than 25% suffer major financial hardship.
The report also found that family physicians, orthopedic surgeons, podiatrists, and physical therapists are keenly aware of this dilemma but often fail to communicate effectively to patients about driving. Most medical professionals express serious concerns about liability regarding return to driving following an injury or surgery. They feel that there is a lack of data to support decisions and inadequate communication among each other. They agree that they must do a better job communicating with patients and their families so they can better prepare for a period of time during their recovery in which they cannot drive.
Recent studies published in the Journal of the American Academy of Orthopaedic Surgeons (JAAOS) and the Journal of Foot and Ankle Surgery (JFAS),determined that there are two significant components in the decision of safely returning to driving after an injury or surgery; the time required for healing and the time required for a return of function. Additionally, it was found that those wearing a surgical shoe or walking boot demonstrated a significantly slower braking response time even in healthy/non-injured individuals wearing the shoe/boot.
During the time required for healing, in addition to the fear of an additional trauma from a motor vehicle accident to the healing body part, there is a general concern about the potential damage that may come from over using the body part to drive before it is adequately healed. For example, a healing fracture in the right lower leg might be compromised or delayed if one must suddenly and forcefully apply the brakes. Also, during this time, it is not unusual for post-injury or post-surgery patients to use pain medications, including narcotics. This will also compromise judgment and reaction time while driving.
Most orthopedic conditions heal in 6 to 8 weeks. However, as many of you may fully know, once a cast or splint is removed, you are not ready to run or jump. Depending on the severity of the injury, it may take many weeks of aggressive physical therapy to regain strength, range-of-motion, agility and dexterity to function at a safe level for a full return to daily activities, including driving.
The current research reinforces the fact that driving safely requires good function of the entire body. For example, just because you broke your shoulder bone but did not fracture your right leg does not mean that you are able to drive safely. Wearing a sling after arm surgery also compromises driving. First, you need a stabilized and healed injury prior to driving. Then, you must work in rehab to make modifications to return to safe driving. Apply the same scenario to injuries or surgery to the spine (neck and lower back).
*Based on research using driving simulators
7 TIPS TO KNOW WHEN YOU ARE READY TO DRIVE:
Remember, every case is unique and there is no substitute for communication with your orthopedic surgeon, podiatrist, family physician and physical therapist.
Visit your doctor regularly and listen to your body.
Keep moving, eat healthy foods, exercise regularly, and live long and well!

EVERY MONDAY – Read Dr. Paul J. Mackarey “Health & Exercise Forum!” via Blog
EVERY SUNDAY in "The Sunday Times" - Read Dr. Paul J. Mackarey “Health & Exercise Forum!” in hard copy
This article is not intended as a substitute for medical treatment. If you have questions related to your medical condition, please contact your family physician. For further inquires related to this topic email: drpmackarey@msn.com
Paul J. Mackarey PT, DHSc, OCS is a Doctor in Health Sciences specializing in orthopaedic and sports physical therapy in Scranton and Clarks Summit. Dr. Mackarey is in private practice and is an associate professor of clinical medicine at Geisinger Commonwealth School of Medicine. For all of Dr. Mackarey's articles, visit our exercise forum!
American Heart Month is not just for lovers. Long after the Valentine’s roses wilt, our hearts will require special attention for a long healthy life. It is the goal of The National Heart, Lung, and Blood Institute to motivate Americans to adopt healthy lifestyles to prevent heart disease.
A recent study by the Center for Disease Control (CDC) found that while many Americans believe that they are “young at heart”, it turns out that many have hearts older than their actual age. For example, the study found that the average American male heart is eight years older and the average American female heart is five years older than their chronological age.
The CDC’s findings may offer some explanation for the fact that many Americans die from heart attacks, strokes, and heart failure when compared to other people around the globe. Furthermore, while more Americans use heart medications more than other people in the world, heart attack and stroke continue to be the leading cause of death in the US, killing more than 80,000 each year.
The CDC has developed a new test to determine “Heart Age,” which has been found to be a much more reliable indicator of a person’s risk for heart disease. The heart age test will determine if your heart is older, younger or average for your age, which can be much more important for longevity than chronological age.
The CDC is encouraging people to take matters into their own hands …be proactive. In addition to calculating your Body Mass Index ((BMI), the CDC is asking people to use an online calculator to determine their heart age. The calculator will give a person a more accurate percentage of risk for heart attack or stroke. Based on the outcome, one must see their family physician or cardiologist to discuss the results and implement a plan.
Heart Age is very easy to use: You just need to enter your age, sex, blood pressure, whether you are treated for high blood pressure, whether you smoke or have diabetes, and your body mass index (BMI), with a handy calculator if you don’t know it. The tool gives you your risk for heart disease in the next ten years, compared with normal.
Visit: www.framinghamheartstudy.org or www.heartfoundation.org
Enter: sex, blood pressure, (list if controlled), diabetes (list if controlled), smoking history, and body mass index (BMI), a simple height/weight calculation found on-line at www.bmicalculator.cc
Example: A 53 year old women with an acceptable BMI, may actually find that she is at great risk for suffering a heart attack or stroke because she smokes cigarettes and has uncontrolled high blood pressure. The calculator includes all the significant factors proven by science to affect a person’s risk of heart attack or stroke. These include: blood pressure, weight, BMI, blood sugar, cholesterol, age, sex and smoking history.
Example: 50 year old male smoker has uncontrolled high blood pressure of 140/96, no history of diabetes, and a BMI of 30 has a predicted heart age of 72 years. A female with a similar profile would have a heart age of 74 years.
To some, the solution may be obvious and for others it may be impossible. In the previous example of the 50 year old smoker, if he quit smoking for one year, he would halve reduced his heart age by 14 years (15 years for a woman). If he would reduce his blood pressure to 120, he would reduce his heart age by 6 years (10 years for a woman). And, if both risk factors were removed, he would reduce his heart age by 19 years (23 for a woman).
In the above examples, the 53 year old man does not have to take his 72 year old heart age as a death sentence.
BY THE WAY…I took the test:
Male: 65
Systolic Blood Pressure: 110
No high blood pressure or diabetes; non smoker
BMI: 22.5
HEART AGE: 62
SOURCES: WWW.CDC.GOV

EVERY MONDAY – Read Dr. Paul J. Mackarey “Health & Exercise Forum!” via Blog
EVERY SUNDAY in "The Sunday Times" - Read Dr. Paul J. Mackarey “Health & Exercise Forum!” in hard copy
This article is not intended as a substitute for medical treatment. If you have questions related to your medical condition, please contact your family physician. For further inquires related to this topic email: drpmackarey@msn.com
Paul J. Mackarey PT, DHSc, OCS is a Doctor in Health Sciences specializing in orthopaedic and sports physical therapy in Scranton and Clarks Summit. Dr. Mackarey is in private practice and is an associate professor of clinical medicine at Geisinger Commonwealth School of Medicine. For all of Dr. Mackarey's articles, visit our exercise forum!